Do That Thing! You Know, the One Thing!
Well, here it is, time to plan. Have you been thinking of what your going to do this year? What changes are you going to make? Also, what did you do this year that you are proud of, that made you happy? Let’s hear it!
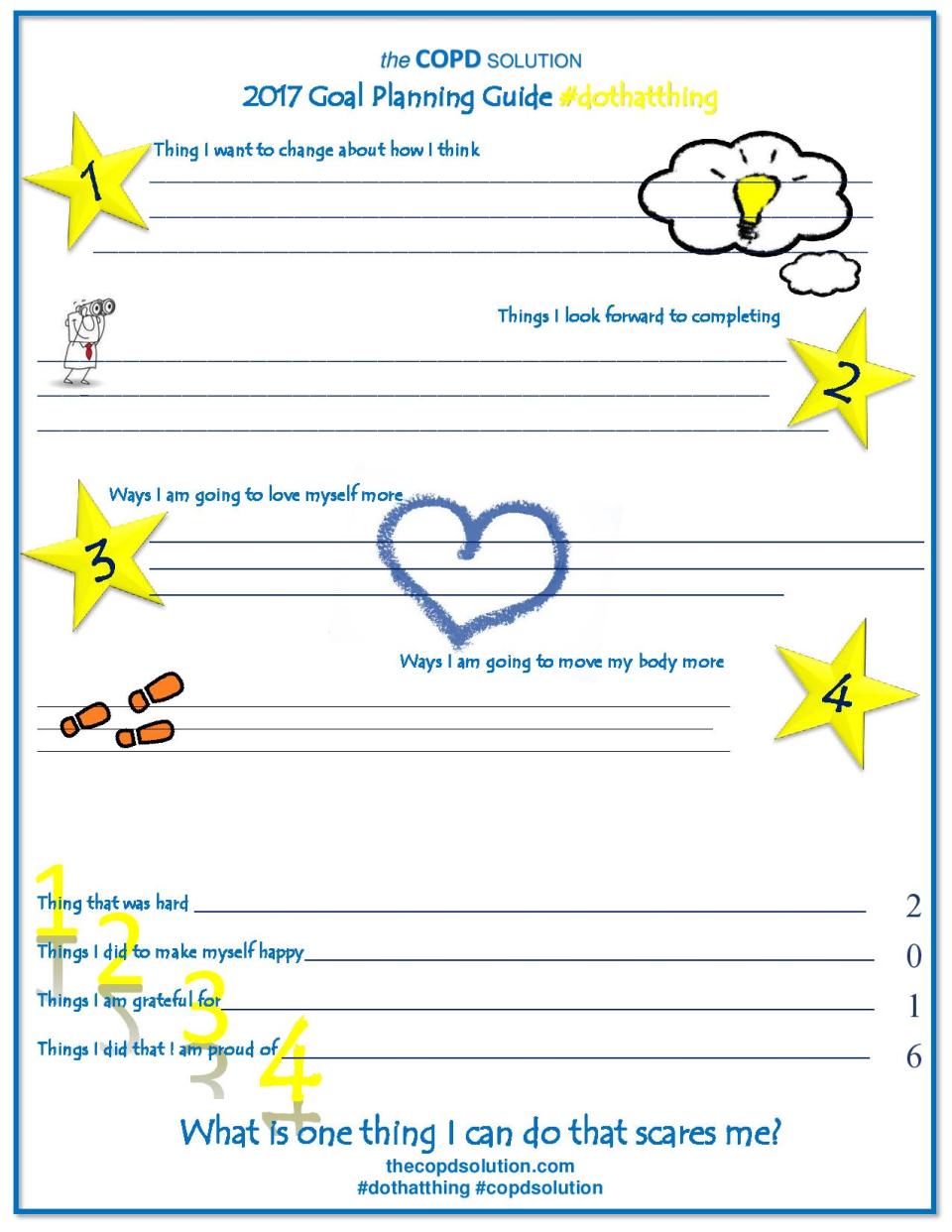
Here is your planning guide… a little thing to give you a little nudge to get to planning, recording, and putting your pen to your thoughts. I have an idea. Let’s plan ONE THING we feel is a crazy thing! I’m not talking jumping out of an airplane crazy, unless that’s your thing, but search inside yourself and find that one thing that makes you scared, and let’s work on it. Maybe you’re scared to share your feelings with someone. Do it. Maybe you’re fear is to wear something new, different. Do it. Or MAYBE you want to go on that vacation you’ve always thought is not possible… how impossible is it? With some planning and work, could you do it? Could you really do it? Look at things with a new set of eyes, a new perspective. Literally, sit or stand differently than you usually do and contemplate things. Hand upside down and watch the flowers grow in the opposite direction. You never know what you may see! #dothatthing will be the way we track what we’ve done, the way we can share what we are doing. Let’s strengthen each other, give courage, and share love! Let’s #dothatthing!
“Do the crazy thing. The hard-to-imagine-but-somehow-you-did thing. The brings-you-to-your-knees thing. The no-one-would-ever-do-it-that-way-thing. The safety-net-would-not-even-matter thing. The it-could-kill-you-but-not-trying-is-another-kind-of-death thing. The thing on your heart. Do it, and let them gasp right before they call it a thing of wonder.”–Ciona Rouse
What’s your thing gonna be THIS year? #dothatthing
Comment below and share, share, share!
Make This YOUR Year to be Your Best You
Happy New Year everyone! Here is hoping happiness and joy were found throughout your holiday season. Hopefully you were able to share with others (our greatest source of joy) and serve someone in some capacity.
As the new year begins it is customary to evaluate where we are and what we can do to improve. So what do you say? Shall we get to it?
Chronic disease can definitely take its toll on those who suffer from it and regardless of which chronic disease you have there are things the sufferers have in common with each other. Which New Years Resolutions will best fit you? Let’s start with a self-evaluation.
There are a few basics we tend to be drawn to when establishing New Years Resolutions. They are popular starting points for many people and for good reason; the basis for those being that self improvement is always necessary and beneficial. Regardless of where we are and what progress we have made the previous year – THERE IS ALWAYS ROOM FOR IMPROVEMENT. These are a few of my personal favorites.
– eating habits
– exercise (aka movement)
– sleep
– meditation
– positive self talk
Eating habits – I don’t know about anyone else but I know that I can always use improvement when it comes to eating habits. I generally do well but every once in a while – far too often – I slip up and my diet for the day is shot. I could even say my diet for the past month has been shot lately! I jumped back on the wagon today, though. A fresh start is in order, and it feels great to be back at it. When you have COPD your diet is very important. What improvements can you make to your daily intake? Can you remove half of you daily sugar intake? How about removing some carbonation? Even better, how about increasing your veggie intake?
Now, how about exercise? Set your goals for incremental increase and start slow enough you can feel the benefits of exercise but not push yourself so hard it actually sets you back when you are recovering. A good rule of thumb I always use tell my patients to remember is to keep themselves at around a level 6-7 for exertion. At this point you should be able to breathe, talk if you HAVE to (but not want to), and tolerate your movement at a pace in which your heart rate is at around 70% of your max. I think a good goal to work toward is one mile each day. This doesn’t mean you have to wake up tomorrow and walk a mile before breakfast. This means you count your steps and throughout the day add them up to equal a mile. What can you do to help yourself get there?
– get up and walk around your house during commercials
– stand in place, holding on to something for stabilization if you need to, and march for three minutes at a time.
– measure a distance in your home or around your home (with good weather you can do this outside, as well) and walk that measured space multiple times each day to help you calculate distance.
– count your steps; it take approximately 2000 steps in one mile. They add up faster than you think!
– it’s also important to remember to set incremental goals for increase. Do a little at a time. You’ll find much more success in taking small steps and increasing as you go.
Sleep is also vital to your success. Rest, rejuvenate, and revive every night. Take tests during the day – there’s nothing wrong with that! Listen to your body and rest when it asks you to. You’ll find you have much more success when you rejuvenate your body with rest.
Meditation is one I am going to focus on this year. Studies show that taking just a few short minutes each day to clear your mind and focus on yourself has measurable benefits to both your physical, mental, and emotional well being. (I will be posting a guided meditation soon, be sure to watch for it!) For starters just find a comfortable position, rest your body focusing on allowing the tenseness in your muscles to leave, close your eyes, and breathe. Listen to the air flow into and out of your lungs. Big inhale through your nose, exhale like your blowing out some candles. Clear your mind, and repeat. Let’s explore and learn this together!
Positive self talk. Do you completely understand the drastic effect this has on your physical well being and how badly negative emotions can have on you? Focus on the positive. Eliminate the negative, (Meditation can also help with this) and tel your self each and every day that you are those things you want to be. Repeat to yourself things like:
– I am strong
– I am healthy
– I am happy
– I am calm
– I can do hard things
– I can handle myself well
– I am successful
– I am good
Why don’t you take a few moments and ponder which areas you feel you could grow and progress in. Write them down – a goal that isn’t written down isn’t really a goal – and see to work on a PLAN to achieve those goals. You will find The COPD Solutions Goal Planning Worksheet in next weeks blog post. Start thinking now so you are ready to fill it out! Let’s achieve together! We should love to hear about your goals AND your progress! Please comment, email, share with us your stories.
Talk soon!
Oxygen Tube Length – What is Safe?
Have you ever wondered what length of tubing is safe for you to use with your home concentrator or portable system? While we have traditionally educated to go no longer than fifty feet, this article from the National Institute of Health cites that even greater length may be effective. Read on to learn “how” this was confirmed.
“Tubing length for long-term oxygen therapy
Aguiar C, et al. Respir Care. 2015.
Abstract
BACKGROUND: Most patients on long-term oxygen therapy use stationary oxygen delivery systems. It is not uncommon for guidelines to instruct patients to use tubing lengths no longer than 19.68 ft (6 m) when using an oxygen concentrator and 49.21 ft (15 m) when using cylinders. However, these concepts are not based on sufficient evidence. Thus, our objective was to evaluate whether a 98.42-ft (30-m) tubing length affects oxygen flow and FIO2 delivery from 1 cylinder and 2 oxygen concentrators.
METHODS: The 3 oxygen delivery systems were randomly selected, and 1, 3, and 5 L/min flows and FIO2 were measured 5 times at each flow at the proximal and distal outlets of the tubing by a gas-flow analyzer. Paired Student t test was used to analyze the difference between flows and FIO2 at proximal and distal outlets of tubing length.
RESULTS: A total of 45 flows were measured between proximal and distal outlets of the 98.42-ft (30-m) tubing. Flows were similar for 1 and 3 L/min, but distal flow was higher than proximal flow at 5 L/min (5.57×5.14 L/min, P<.001). FIO2 was lower at distal than proximal outlet tubing at flows 1, 3, and 5 L/min, but the mean difference between measurements was less than 1%.
CONCLUSIONS: Tubing length of 98.42 ft (30 m) may be used by patients for home delivery oxygen with flows up to 5 L/min, as there were no important changes in flows or FIO2.
Copyright © 2015 by Daedalus Enterprises.
Bottom Line Health
Hello everyone! We would like to share with you an article with contributions by our author that has been utilized by Bottom Line Health, an industry leading health magazine. If you haven’t seen it yet, you should. You can find more information about subscribing to the magazine here at
You will find it full of information for all aspects of your health and wellness, all geared toward you and what you need!
Dawn’s specific COPD article can be found following this link. It had such great results it is now available to everyone – not just paying subscribers – on their website. We hope you enjoy it!
Dr Rebecca Risk Radio Show
We were excited to be a part of Dr Rebecca Risk’s Radio show this morning! It was a great conversation and a good time talking with her about chronic lung disease and how to help it. Take a listen and hear for yourself! 🙂
It’s Virtual Lobby Week!
Let your voice be heard! Click here to show your support:
http://c.aarc.org/advocacy/lobby_week/
What do you need to know about HR2948 – the Medicare Telehealth Parity Act?
If enacted it will be implemented over three phases, each two years apart.
The first phase includes
- Covering RTs as qualified telehealth providers (along with certified diabetes educators, physical therapists, occupational therapists, speech-language pathologists, and audiologists.
- Incorporates respiratory therapists in the Medicare statute, something AARC has strived to achieve through its previous legislative initiatives.
- Includes coverage of respiratory services, audiology services, and outpatient therapy services including PT, OT and SP.
- Adds remote patient monitoring (RPM) for patients with COPD and heart failure and related comorbidities when provided under chronic care management.
- Expands telehealth coverage to any Rural Health Clinic and Federally Qualified Health Clinic and metropolitan counties with populations fewer than 50,000, including use of store and forward and video conferencing.
Second phase includes
- Adding an individual’s home as a telehealth site related to hospice care, home dialysis, eligible outpatient mental and behavioral health services, and home health services which include outpatient therapy services and durable medical equipment.
- Expanding telehealth access to evaluate/treat acute stroke regardless of patient’s location.
- Expanding telehealth coverage to metropolitan counties with populations of 50,000-100,000, including store-and-forward and video conferencing technologies.
- Adding remote patient monitoring for patients with diabetes and related chronic comorbidities when provided under chronic care management.
- Requires a report on the effectiveness of new telehealth services and providers with respect to patient satisfaction and responsiveness to needs/concerns.
Third (and final) phase includes
- Expanding telehealth coverage to metropolitan counties with populations greater than 100,000, including store-and-forward and video conferencing technologies.
- Adding remote patient monitoring for other chronic conditions/related chronic comorbidities specified by the Secretary when provided under chronic care management.
What is telehealth, remote patient monitoring, and store and forward technology? How do they work?
- Telehealth is an interactive audio and video telecommunications system which allows real-time face-to-face communication between physicians and other health care providers and their patients located at different sites. For example, the beneficiary may be physically located in a rural health clinic or a skilled nursing facility while the physician is in his/her office suite or the hospital. The term “telemedicine” is often used interchangeably with “telehealth.”
- Remote patient monitoring is conducted via a coordinated system that uses one or more home-based or mobile monitoring devices that automatically transmit vital sign data or other information as part of a patient’s plan of care wirelessly, or through a telecommunications connection to a server, allowing review and interpretation of that data by a health care professional.
- Store-and-Forward Telehealth involves the acquisition and storing of clinical information (e.g. data, image, sound, video) that is then forwarded to (or retrieved by) another site for clinical evaluation (e.g., analogous to sending a picture via text message). For Medicare, this means the information would be transmitted from the originating site where the beneficiary is located to the distant site where the physician/practitioner is located for review at a later date.
These are exciting changes! What does Medicare currently cover with regards to these services?
Medicare’s currently coverage of telehealth services is limited to rural counties and health shortage areas in metropolitan fringes with the patient at a health facility (known as “originating sites). Originating sites include physician offices, hospitals, skilled nursing facilities, and rural health clinics. Practitioners who can provide telehealth services currently include physicians, nurse practitioners, physician assistants, nurse-midwives, clinical nurse specialists, clinical psychologists, clinical social workers, and registered dietitians or nutrition professionals. Only a select number of medical procedures/services are covered such as consultations, counseling services, education, patient assessments, smoking cessation and transitional care management services.
Remote patient monitoring and store-and-forward technologies are not covered under Medicare’s telehealth rules.
What is a qualified respiratory therapist?
The Act does not specify qualifications for any of the newly covered providers. Those details will be left up to local contractors to determine, and will allow those contractors (physician or facilities) to bill Medicare directly for the telehealth services furnished by RTs.
Telehealth services are an integral part of a growing healthcare system and continue to gain recognition and attention of Congress. There are several initiatives currently underway with a focus on telehealth and remote patient monitoring, and there could be more to come in future sessions. The AARC supports the expansion of telehealth and remote patient monitoring, especially advocating HR2948 because it includes coverage for RT services and allowing our profession to serve as telehealth providers. Although there has been no formal cost estimate made, the Congressional Budget Office has performed an informal analysis of telehealth and consider two main issues. The first being payment rates that would be established for telehealth services, and the second being whether telehealth services would be a substitute for other Medicare-covered services or would be used in addition to currently covered services. Cost and/or savings depend on the second issue and the specific provisions of the bills. Further study would be of benefit with results of a well-designed study examining the benefits of how these services would affect health care expenses in this patient population.
We need your support!
There are numerous reasons as to why this Act is important to our profession and why your support is needed. Such as:
Recognizing RTs as health care providers in the Medicare statute which has been a long-standing goal of the AARC.
- Recognizing the importance of respiratory services by covering them as part of telehealth.
- Enhancing the ability of RTs in providing a comprehensive disease management program to their patients to prevent acute exacerbations.
- Permitting RTs to evaluate or manage patients via remote patient monitoring (RPM) as long as the patient is receiving other chronic care management services.
- Offering a new way to deliver respiratory services that are currently not available to RTs as part of the Medicare program.
- Expanding the location of originating sites (reaching patients who suffer from chronic respiratory disease that can be helped by respiratory therapists).
- The bill has bipartisan support, having been introduced by Representatives Mike Thompson (D-CA), Greg Harper (R-MS), Diane Black (R-TN) and Peter Welch (D-VT).
- AARC would not be the only organization lobbying Congress for sponsorship of the bill; we would be part of number of influential organizations whose goal is to increase the ability of Medicare patients to receive telehealth and RPM services.
- It is the only telehealth bill that specially includes respiratory therapists and respiratory services in statutory language.
- It provides Congress with a report that has the potential to highlight the value of RTs and other providers in how they meet the needs of their patients.
Please click on the link at the top of this page to send your letter of support for this important legislation. It will take only a moment of your time and make a world of difference to our future.
So, Pneumonia Set In…
I have had an interesting week this past week. I got this nagging cough that wouldn’t go away. It kept getting worse and worse… So, I went headed to the Dr. That’s right… pneumonia, it was. While I was struggling, achy, and all the good stuff that goes with it, I was struggling to breathe, but not TOO bad, at least not yet. The real trouble came when I went home.
I left the office and headed toward home to rest before getting my prescriptions filled. I was tired. And achy. Did I mention achy? Well, while I was there, laying on my heating pad popping Ibuprofen 800s and trying to gather the energy to run to the pharmacy, my wheezing worsened. And worsened. Pretty soon a simple breath resembled the sound of that freight train I heard enter the sugar factory earlier in the week. So, I decided that whether I felt energetic enough to get up and go to the pharmacy or not, I needed to.
Stepping outside didn’t help. Have you read the news about Utah’s latest inversion and our air quality? It’s worth mentioning. It’s HORRIBLE! It is this mucky, thick, brown-tinged air that belongs nowhere it could possibly be inhaled by anything. It’s bad, really bad. Worst in the nation, I believe I just read. Needless to say, inhaling that toxicity did nothing but worsen my ability to breathe. About halfway to the pharmacy I noticed my face started to feel numb along with the end of my nose. Nervous at this thought, I pulled out my oximeter and placed it on my finger. Waiting for it to calibrate my heart rate and oxygen levels jumped around a bit, only to settle on what is a HORRIBLE reading for me… heart rate of 107, SpO2 of 69. I told my husband to drive faster. I needed that inhaler in a bad way. Let’s just say I ended up on oxygen, obviously, with a nebulizer (to be used every four hours) and a good dose of antibiotics.
Long story short, I’m feeling better, finally. Days later. I will return my oxygen tomorrow, I will soon return to my own “normal” energy levels, and all will be well, I’m sure, but in the meantime it was sobering to feel so short of breath and have to use all my accessory muscles to do so. I thought of you, all of you. And I was reminded of the strength and power you all have within you and of that strength, evident in the eyes of those who have it. Look in your own mirror each morning. Look for that power. It’s there, beneath the doubts. It’s there. You have it and you are an inspiration to the world! Thank you for sharing it with us.
Happy Breathing!
ALA Lung Force Expo
 Do you know about the American Lung Associations Lung Force Expo? It’a going to be a great opportunity for patients and families alike to learn, speak with professionals, and find the support and resources you need to manage your disease. We will be at the Expo located in Salt Lake City, UT, USA, but if you are in the United States there’s one near you!
Do you know about the American Lung Associations Lung Force Expo? It’a going to be a great opportunity for patients and families alike to learn, speak with professionals, and find the support and resources you need to manage your disease. We will be at the Expo located in Salt Lake City, UT, USA, but if you are in the United States there’s one near you!
Check it out here! http://action.lung.org/site/TR?pg=entry&fr_id=14169
Want to learn more?
Norwex… cleaning and disinfecting without any fumes
I received from my dear mother-in-law, for Christmas, some Norwex products. I had heard about these products and seen them for sale at various locations, but have never actually tried them. I must admit, I had my doubts that they were as “awesome” as they were said to be…. but my mother-in-law is a trustworthy woman, so I had to try.
I have the dusting mitt, which is blue, and the glass rag, which is purple. (after you visit the web site the colors will mean more to you.) I tried the dusting mitt first. It worked amazingly well at picking up the dust of all types of surfaces, and I noticed it seemed to really prevent the dust particles from flying around in the air. I dusted my whole house, floor to ceiling, upstairs and downstairs, with the mitt. It worked well.
It worked so well I decided to try the glass rag. I wanted to try it first in my kitchen, on the microwave, ovens, and fridge. The microwave was what I cleaned first, and I did this on purpose, as it is positioned over my stove top and likes to collect grease from anything that is cooked on the stove top. I thought this would be a good product test. It cleaned it, with very little elbow grease, to sparkling with only water sprayed on the surface. The rest of the kitchen sparkled as well as the microwave by the time I was done, so I moved onto the bathroom mirrors. Now, we have six children. Five of them are boys. That is a lot of toothpaste, hair gel, fingerprints, etc on the bathroom mirror so I chose the main kids bathroom to clean first. Needless to say, all the bathroom mirrors sparkled just as much as the microwave by the time I was done, even though I was using the same rag I had already cleaned the kitchen with, and I had only used water sprayed from my spray bottle on the various surfaces. ( I continued to clean all windows in my house that could be reached without a ladder. They all cleaned very well, no streaking or marks, and no window cleaner was used at all.)
Anyway, as I was using these rags, I though of all my lung friends, and the struggle I have heard time and time again of cleaning fumes and the irritations they tend to cause. I got a little excited, as I tend to do whenever I find anything that I think may be helpful, and had to test the product to the max prior to sharing my opinion with you all, but now that I have done so, and “this house is clean”, I can honestly say that this product is something that you may want to check out.
The products are sold via distributors, so I have included the web site here, in hopes that it will direct you to a distributor in your area. If it does not work, please let me know and we will do what we can to find someone to help you.
Let us know what you think, if you try it, and how it goes! Much love to you all. We will be waiting to hear…
Introducing The COPD Solution, Understanding, Living & Breathing Better with Lung Disease
The COPD Solution was written and designed by a lung disease expert for patients just like you. As a comprehensive program designed to fully transform the day to day life of a patient with chronic lung disease, it fits into the complicated and often difficult situation that patients find themselves in when lifestyle modification becomes a “must do”. Proven through hands on use with hundreds of patients, this program has experienced a 100% success rate showing marked improvement in an increased mental, physical, and emotional well being of those who fully participated. Life sometimes throws us situations and challenges that seem overwhelming. The COPD Solution can help you recognize, change, and live with your difficult situation. Check out our testimonials page for a quick overview of some of our success stories.
